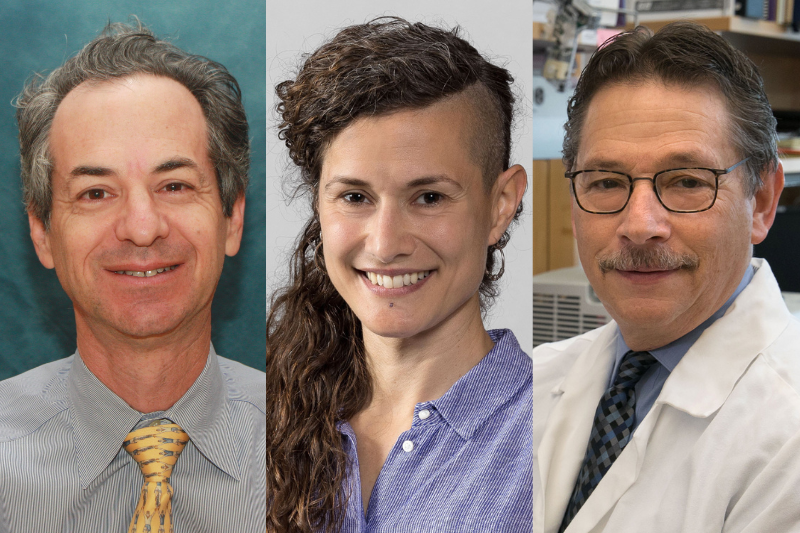
From left to right: Dr. Gerald Lipshutz, Dr. Zulema Romero Garcia and Dr. Donald Kohn
Researchers at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA have received more than $16 million in grants from the California Institute for Regenerative Medicine, the state’s stem cell agency, to advance new stem cell-based treatments for a metabolic disorder and two rare genetic immune disorders.
The grants, awarded to Dr. Gerald Lipshutz, Dr. Zulema Romero Garcia and Dr. Donald Kohn, are part of the CIRM Therapeutic Translational Research Program, which aims to get projects ready to enter clinical study.
Gene therapy to treat arginase deficiency
Dr. Gerald Lipshutz, professor of surgery and molecular and medical pharmacology
Lipshutz’s $5.3 million award will fund his work to develop a gene therapy to treat arginase deficiency, a metabolic disorder that causes the amino acid arginine, ammonia and abnormal metabolites called guanidino compounds to build up in the blood and brain. Patients with the inherited disorder typically appear healthy at birth but start to show signs of progressive developmental delays, cognitive decline and mobility impairment between the ages of 1 and 3. Current treatments focus on strict dietary control, including restriction of protein intake, but are minimally effective and almost always unable to prevent disease progression. Lipshutz and his team aim to develop a viral vector-based gene therapy that will produce the missing or deficient arginase protein in the liver, which will restore the body’s ability to break down arginine and ammonia, as well as prevent the accumulation of guanidino compounds. If shown to be safe and effective in a future clinical trial, this potentially curative treatment could shift the paradigm by which arginase deficiency is treated.
New gene editing approach for CD3 delta severe combined immunodeficiency
Dr. Zulema Romero Garcia, assistant adjunct professor of microbiology, immunology and molecular genetics
Romero’s award of $6 million will support her efforts to develop a safer and more efficient gene therapy treatment for the rare and deadly genetic condition CD3 delta severe combined immunodeficiency, or CD3 delta SCID, using a precise genome editing technique called base editing. The disease is caused by a mutation in the CD3D gene that prevents blood stem cells from producing T cells. Due to the lack of T cells, babies born with this condition are unable to fight off infections and if untreated, often die before the age of 2. Romero and her collaborators are working to bring a base editor that is highly efficient at correcting the disease-causing genetic mutation to clinical trial. This novel platform holds the potential to not only transform treatment options for patients with CD3 delta SCID but also to create a pathway to treat other inherited disorders. This project has received previous funding from the Jeffrey Modell Foundation.
Gene editing to treat X-linked agammaglobulinemia
Dr. Donald Kohn, distinguished professor of microbiology, immunology and molecular genetics and of pediatrics
Kohn’s $4.8 million award will fund his work to develop a gene therapy for X-linked agammaglobulinemia, an inherited immune disorder that prevents the body from making infection-fighting antibodies. Without antibodies, people with the disorder—who are almost exclusively male—often develop severe, recurrent bacterial infections of the ears, internal organs, sinuses, bloodstream and skin. Patients currently require costly monthly injections of antibodies to prevent infections or reduce infection severity. However, Kohn and his team are preparing to bring a gene therapy to clinical trial that can serve as a one-time treatment by correcting the mutations in the Bruton’s tyrosine kinase gene function and enabling the body to properly produce antibodies. This research has been supported by a previous award from the CIRM Discovery Program. The project has also received funding from the Immune Deficiency Foundation.
The therapeutic approaches described in this article have only been used in preclinical tests and have not been tested in humans or approved by the Food and Drug Administration as safe and effective for use in humans.
Linda Wang
(310) 429-9102
linwang@mednet.ucla.edu
